Children &COVID-19 &Diagnosis &IPTp &ITNs &Malaria in Pregnancy &Treatment Bill Brieger | 06 Oct 2022
2021 DHS and MIS Findings from Six Malaria Endemic Countries
The Demographic and Health Survey Program has released final and summary reports for both DHS and Malaria Indicator Surveys (MIS) for 2021 from several malaria endemic African countries. Below is a brief summary of some of the findings from Madagascar, Nigeria, Burkina Faso, Mali, Côte d’Ivoire, and Senegal. Click the link on each country to download a copy for yourself.
The proportion of the population who slept under an insecticide treated bednet the night before the survey varied. In Madagascar it was 49%, While in Nigeria it was 59%. Mali achieved the highest coverage at 73%, while Burkina Faso had the lowest previous night coverage at 41%.
 Senegal showed a worrying decrease from 63% in 2016 to 46% in 2021. Côte d’Ivoire did not report total household use, but indicated that 72% of homes had at least one net, with 58% of children below 5 years of age and 64% of pregnant women sleeping under them.
Senegal showed a worrying decrease from 63% in 2016 to 46% in 2021. Côte d’Ivoire did not report total household use, but indicated that 72% of homes had at least one net, with 58% of children below 5 years of age and 64% of pregnant women sleeping under them.
At least three doses of sulfadoxine-pyremethamine is recommended for Intermittent preventive treatment of malaria in pregnant women. The national average was 38% for at least 3 doses in Senegal, although ironically 92% had been reached with the first dose. In Mali only 35% received at least a third dose. Burkina Faso started out with 92% for the first dose, but reached 57% with three or more. Côte d’Ivoire started with 80% receiving their first dose and concluded with only 35% receiving a third. Both Madagascar and Nigeria had the lowest 3-dose coverage at 31%.
Malaria testing and treatment using rapid diagnostic tests and artemisinin-based combination therapy (ACT) was reported. Nigeria demonstrates the challenges of following guidelines. Although 63% of children under 5 years of age were reported to have had a fever in the two weeks preceding the survey, only 24% of those received a diagnostic test. The summary results report that 74% of those with fever “who took any anti-malaria medicine” used the recommended ACT. The implication is that many received medicine without confirmatory testing such that some may have gotten ACT who needed another medicine and some who actually had malaria may have missed the correct treatment.
 A similar low level of testing was seen in Senegal (22%), Mali (23%), and Madagascar (20%). Côte d’Ivoire reported 38% of febrile children having been tested. Burkina Faso performed better for testing with 65%.
A similar low level of testing was seen in Senegal (22%), Mali (23%), and Madagascar (20%). Côte d’Ivoire reported 38% of febrile children having been tested. Burkina Faso performed better for testing with 65%.
These brief findings indicate that implementation of Malaria interventions are far from ideal. We know that some of the blame can be placed on health service disruptions due to demands of COVID-19 activities by health ministries and partners. Still, with 8 years remaining until 2030, Reinvigorated efforts are needed in all endemic countries if these six examples are indicative of the challenges we face.
 (Graphic source: https://www.aafp.org/news/health-of-the-public/20210429vacchesitancy.html)
(Graphic source: https://www.aafp.org/news/health-of-the-public/20210429vacchesitancy.html)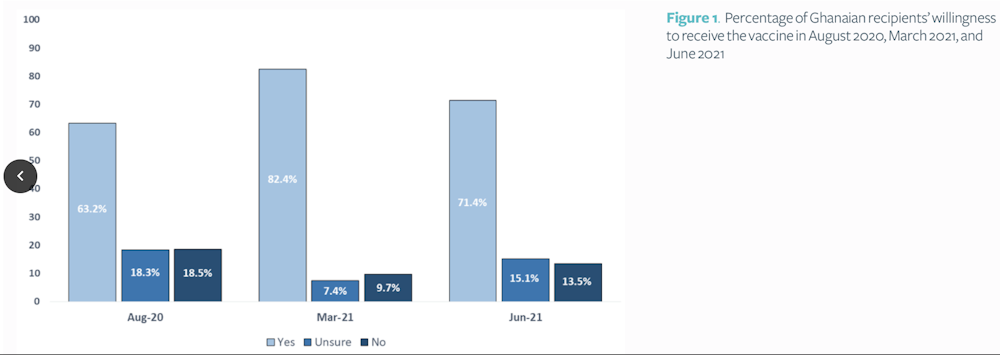
 Adapted from
Adapted from  Dengue has been endemic in Singapore for many decades, with all four dengue serotypes (DENV-1-4) in active circulation.
Dengue has been endemic in Singapore for many decades, with all four dengue serotypes (DENV-1-4) in active circulation. 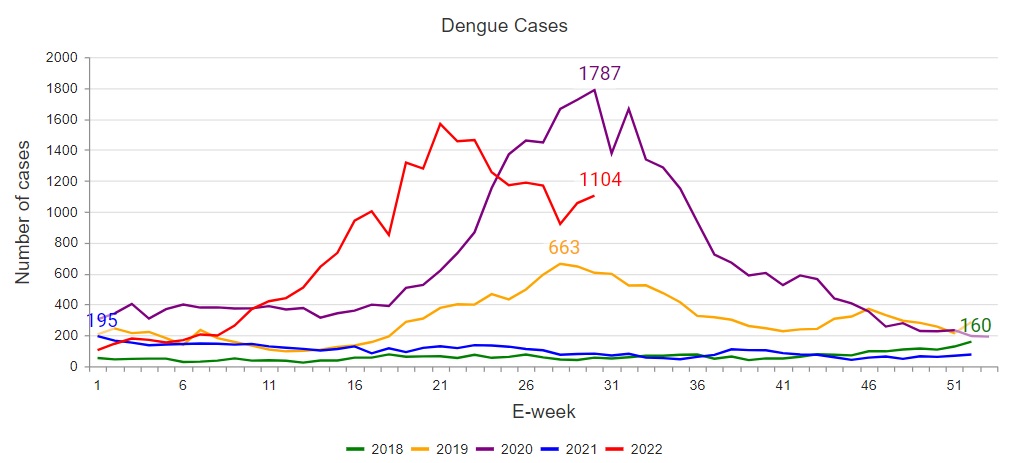
 average Singaporean. (Vaccine Photo credit: http://bitly.ws/twGk).
average Singaporean. (Vaccine Photo credit: http://bitly.ws/twGk).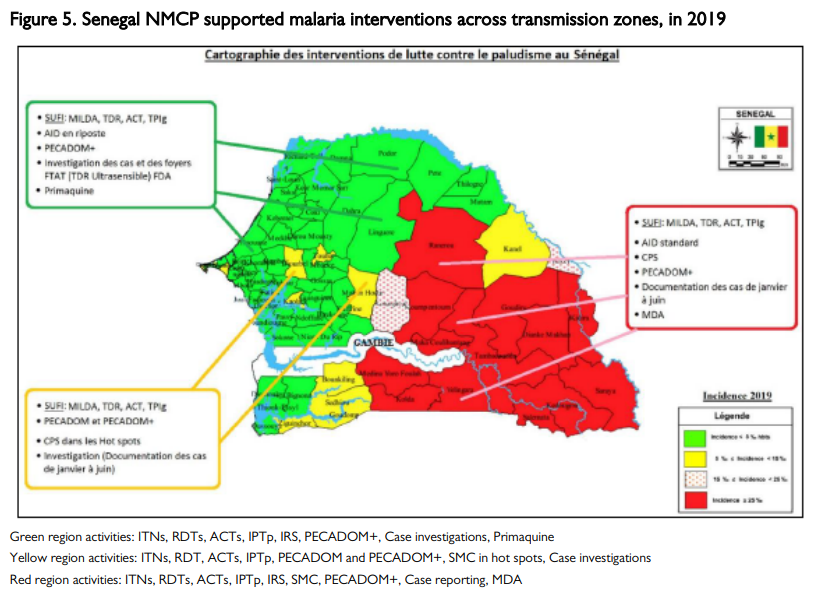 Although malaria transmission and infection rates in Senegal have declined in the past two decades from over
Although malaria transmission and infection rates in Senegal have declined in the past two decades from over  The
The 







