Ebola Bill Brieger | 10 Mar 2020 02:12 pm
Lessons Learned from Ebola Management in Sierra Leone
Lessons can still be learned from the Ebola experience in West Africa. Daniel Ehrenpreis and Masahiro Katahira as members of the class, Social and Behavioral Foundations of Primary Health Care, have posted a blog on the importance of financing at the local government level to ensure better disease control efforts. Their thoughts are posted below.
In 2015, Sierra Leone experienced the height of the Ebola epidemic, where there were over 13,000 confirmed cases; 29% of which were fatal. The prolific nature of this disease made controlling the spread difficult to manage. The government of Sierra Leone initially coordinated the Ebola mitigation efforts by allocating funding to centralized approaches . This method quickly became ineffective as the virus rapidly proliferated and mortality skyrocketed. Different Ebola response efforts were needed to curb the spread of this infectious disease.
While many international organizations were funneling funding into national response measures, localized infection control interventions were being undermined. This created uncoordinated Ebola control measures that exacerbated the virus’ mortality rate. Furthermore, localized non-governmental organizations (NGOs) were disproportionately underfunded and thus did not have the resources to implement effective Ebola mitigation techniques.
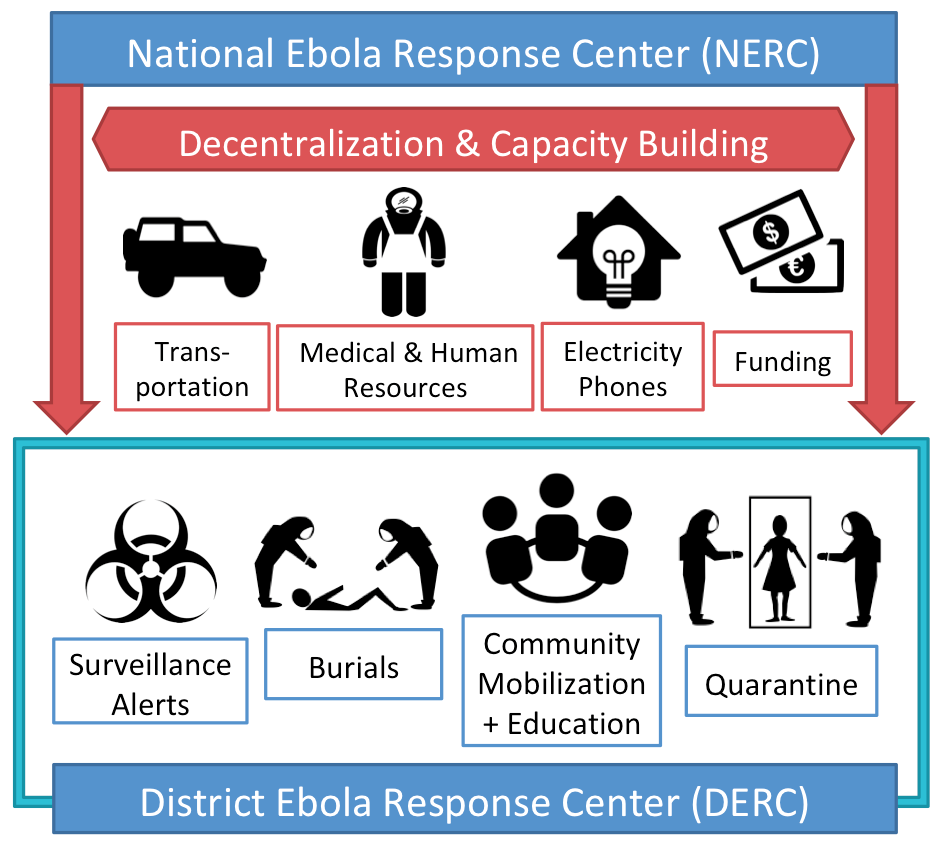
The National Ebola Response Center (NERC) consisted of the army of Sierra Leone and England, including international agencies such as, UNMEER, WHO, and CDC. All 14 districts of Sierra Leone had a District Ebola Response Center (DERC). (See Figure #2)
The DERC had localized roles, such as surveillance, alerts, burials, community mobilization & education, and quarantine. Low capacity of district health infrastructure and insufficient funding challenged DERCs and local NGOs. With a lack of medical resources including protective clothes due to their poor logistics system, reduced communication between staff in the NERC due to no electricity, distrust from community members, and an inadequate number of staff, there were many barriers preventing the success of localized Ebola response. Also, since every DERC had to meet the needs of different communities, the DERCs did not always act in alignment with the NERC’s plan. It was clear that more funding and resources were needed in the DERCs.
To respond effectively to future Ebola epidemics, national governments should consider allocating funding from both internal finance and international donors to decentralized health management approaches. The 2015 Ebola epidemic in Sierra Leone exemplified the need to strengthen local health sectors, and it is the responsibility of national policymakers to bolster the capacity of our localized health systems for effective control and response.
